Real User Stories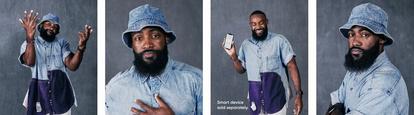
‘Do You Want to Live?’: One Warrior’s Turning Point in Life with Type 1 Diabetes
Oct. 18, 2024 • 5 min read
For some people with diabetes, there comes a moment of reckoning where the body forces them to take their management more seriously. Dexcom Warrior Steven Cannady, 32, of Durham, North Carolina, has weathered several.
One afternoon in his mid-20s, he fell to the floor of his apartment, knocking over a glass of Kool-Aid from a table. He woke up sucking the Kool-Aid from the carpet in a panicked effort to stay alive. He once drove to work and woke up on the side of the road unable to recall the five-mile trek and had to call for help. Then there were two bouts with diabetic ketoacidosis (DKA) and a serious “scared-straight” talk with a doctor.
Steven’s evolution from a self-described “weird and shy kid” who didn’t take his diabetes management as seriously as he should into a healthy Dexcom Warrior who travels the world began over a box of cereal just before Christmas when he was 13.
Diagnosis and stubbornness
On Dec. 21, 2004, Steven spent the day happily in front of the TV eating Froot Loops. But he soon grew concerned when he had to visit the bathroom every 15 minutes or so. As the day progressed, his thirst became unquenchable. Later that evening, he could barely walk and ended up lying on the kitchen floor shivering even though his body felt hot. His mother got home from work and immediately rushed him to the emergency room, where for several hours they tested him as he continued to frequent the bathroom. Ultimately, the staff checked his ketones and glucose and diagnosed him with Type 1 diabetes after finding his glucose was above 700 mg/dL.

“I didn’t know what diabetes meant,” Steven said. “I knew it had something to do with sugar, but that’s really all I knew. And then they tried to explain, ‘You’re going to need to do this and do that,’ and I developed a sense of fear, like, ‘I have to inject insulin, prick my fingers and I have to do what?’”
He left the hospital Christmas morning and spent the next week with family taking classes to learn how to check his glucose levels, how to inject insulin and master the other finer points of proper diabetes management. He stayed on top of things for about a year, but he hated the fingerpricks and quickly began to avoid them.
“Around my sophomore or junior year of high school, I was just at a point where I didn’t check my glucose that often,” he said. “I wasn’t taking my medicine. I didn’t care about diabetes. I wanted to eat what I wanted to eat. I wanted to do what I wanted do. I’d just visit the school nurse if I felt bad or guesstimate my insulin before eating, but I never really knew my numbers.”
He remained an active member of the school track team and played basketball recreationally, but his failure to properly manage his Type 1 diabetes caught up to him with two rounds of DKA. That’s when a doctor at Duke Health read him the riot act.
“She just straight up told me, ‘Hey, you’re 16. Do you want to live?’” Steven recalled. “’Do you want to have kids and see your kids? Do you want to run track? Do you want to keep playing basketball? Do you want me to cut off your toes or legs? Do you want to go blind?’ And I was like, ‘Whoa, chill out!’ And she said, ‘Yeah well, this is the path you’re going to be on unless you start taking this more seriously.’”

Old habits face an ultimatum
In college at North Carolina Central University, he often introduced himself as “My name is Steven with diabetes” and became known for his outgoing personality, active involvement in campus life and his diabetes. But like most college students, Steven lived on a tight budget and he often neglected his management, rationing insulin he got from student health and focusing more on his social life rather than a healthy lifestyle.
After graduation, not much changed in his diabetes management. As a result, his girlfriend Nia (now his wife) and his friends got into the habit of “shoving apple juice down my throat” when his glucose got too low.
“I’ve had her, I’ve had friends, I’ve had frat brothers – a lot of people have saved my life because my sugars got low,” he said.
While everyone with diabetes needs a support system, his family and friends grew concerned and frequently encouraged him to take better charge of his self-care. Nia, who got a job in clinical research, told him about the Dexcom continuous glucose monitoring (CGM) system about five years ago. Soon after, the CFO of a church where he worked as a contractor told him about his daughter, who lives with Type 1 and uses Dexcom CGM. While offering him a new full-time position, his boss made it a stipulation that Steven had to get a Dexcom G6 if he wanted the new job.
He relented. And since then, his life has never been the same.
Dexcom CGM makes the difference
“For one, no more fingersticks,”† he said. “Second, it’s the peace of mind because of the alerts. Around that time, my levels were super low a lot probably because, again, I was just kind of guesstimating my insulin. Most days if I played basketball, I ran track or I did something active cardio-wise, I took the same amount of insulin not knowing that if I took a nap, my levels would drop, which is probably what happened a lot of those times. But Dexcom CGM just changed everything.”
†Fingersticks required for diabetes treatment decisions if symptoms or expectations do not match readings.

Having real-time data has empowered Steven to take active control of his management and live a life with more certainty about how his diabetes impacts him.
“I can look in real time and see these are my numbers,” he said. “And I know my levels at all points in time. So even if I’m about to go to sleep at night, then I’ll drink some juice before I go to sleep. But if I am asleep, if my sugar is so low, I’ll get an alert on my phone. My wife wakes up or I wake up and take care of it.”
Now coming up on one year as a Dexcom G7 user, Steven raves about the upgraded, smaller technology and how it makes it even easier to manage diabetes.
“It only takes about 30 minutes to warm up, versus two hours with Dexcom G6, which is great,” Steven said. “Then the 12-hour grace period to change sensors is probably my favorite part. It’s amazing because sometimes I might be at work and my sensor expires or I might be out and my sensor expires, but I have more time to change it. And then whenever I do change it, 30 minutes is not going to affect my glucose levels significantly. Nothing crazy is going to happen in about 30 minutes.”
Today, his A1C is around 6.4%* and his endocrinologist has noticed a big difference in his health.
“The visits are much quicker, in and out,” Steven said. “Everyone can tell the difference. And just having that peace of mind to know how certain things really affect my levels so that I’m more aware about it. It’s life-changing! You can’t pay for peace. It makes you aware of literally everything. Food, how you work out, what juice does.”

With more peace of mind, Steven can focus more on the things he enjoys most in life. He has a blossoming career in workforce development and recruiting for the booming biomanufacturing and biotechnology industries in North Carolina’s Research Triangle Park. And he and his wife are avid world travelers who recently toured Turkey and Italy and are now planning a long summer vacation that will begin in Greece and take them to Paris for the 2024 Summer Olympic Games.
Thanks to Dexcom CGM, he’s looking forward to trying new foods across Europe while feeling confident in knowing how they’ll impact his levels. In fact, other travels have enlightened him to how much healthier food can be outside the United States.
“The crazy thing is the food over there is actually lower in sugar, which I had to learn the hard way because I’m used to taking the same amount of insulin I take when I eat whatever foods,” he said. “I go over there and even though I eat a croissant or something, there’s been plenty times where my levels have been low because I thought, ‘Oh, it’s a croissant, or it’s the jelly.’ Overseas, I also know that these certain foods won’t do the same things to my body because the food quality is just a lot better.”
And as a Warrior, he looks forward to when people on the streets ask about his Dexcom CGM on his arm – whether in Durham or abroad.
“I make a lot of friends,” he said. “When I’m out, I get stopped, people see me with a Dexcom G7 on my arm, or I might see them with one on their arm and they’ll ask me questions. Either ‘What is that?’ Or ‘Hey you, hey diabuddy!’”
Steven takes it all in stride, knowing he could help someone else better understand diabetes or find their own breakthrough in their diabetes journey.
Individual results may vary
BRIEF SAFETY STATEMENT: Failure to use the Dexcom Continuous Glucose Monitoring System and its components according to the instructions for use provided with your device and available at https://www.dexcom.com/safety-information and to properly consider all indications, contraindications, warnings, precautions, and cautions in those instructions for use may result in you missing a severe hypoglycemia (low blood glucose) or hyperglycemia (high blood glucose) occurrence and/or making a treatment decision that may result in injury. If your glucose alerts and readings from the Dexcom CGM do not match symptoms, use a blood glucose meter to make diabetes treatment decisions. Seek medical advice and attention when appropriate, including for any medical emergency.
Dexcom, Dexcom Clarity, Dexcom Follow, Dexcom One, Dexcom Share, and any related logos and design marks are either registered trademarks or trademarks of Dexcom, Inc. in the United States and/or other countries. ©2023 Dexcom, Inc. All rights reserved.
